Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Multiple Sclerosis Rehabilitation
Multiple Sclerosis Rehabilitation is a process that helps a person achieve and maintain maximal physical, psychological, social and vocational potential, and quality of life consistent with physiologic impairment, environment, and life goals. Achievement and maintenance of optimal function are essential in a progressive disease such as MS.
Definition Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic inflammatory, demyelinating disease of the central nervous system (CNS). It affects largely young adults between the ages of 20-50, and is often reffered to as the " great crippler of young adults ".
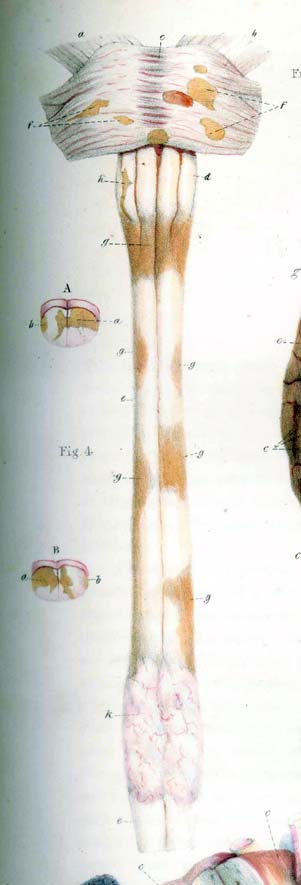
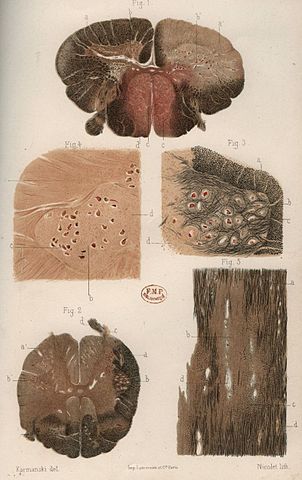
History of Multiple Sclerosis
Multiple Sclerosis was described as early as 1822 in the diaries of an English nobleman and further depicted in an anatomy book in 1858 by a British medical illustrator. Dr. Jean Cruveilhier, a French physician, first used the term "islands of sclerosis" to describe areas of hardened tissue discovered on autopsy. However, it was Dr. Jean Charcot in 1868 who defined the disease by its clinical and pathological characteristics: paralysis and the cardinal symptoms of intention tremor, scanning speech, and nystagmus, later termed Charcot's triad. Using autopsy studies he identified areas of hardened plaques and termed the disease sclerosis in plaques.
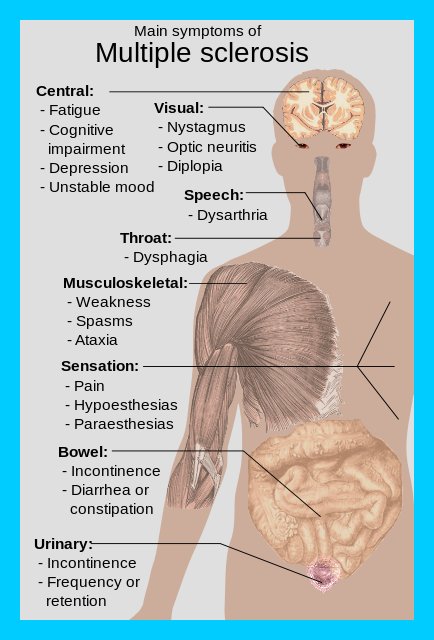
Early Symptoms of Multiple Sclerosis
Usually this first symptoms of MS are tingling and numbness in the face, hand and feet, as well as vision problems. As the disease gets worse, symptoms such as shaky movements, walking problems, difficulty with movements and sensation, bowel and bladder control problems, and feelings of exhaustion develop.
Many people with MS have weeks where they have these symptoms and then years where they are symptom free and feel fine. As the disease progresses the times where they do have symptoms, gets longer and worse and they do not return to normal following the attack.
Multiple Sclerosis Rehabilitation can help people with MS after they have had an attack, help to educate them how to prevent other complications from occurring, and help teach them how to compensate for changes that may not get better. They can also help direct them to MS organizations in their community.
The Role of Multiple Sclerosis Rehabilitation
The goal of rehabilitation is to improve and maintain function. From the time of diagnosis onward, Multiple Sclerosis Rehabilitation specialists provide education and treatment designed to promote good health and general conditioning, reduce fatigue, and help you feel and function at your best—at home and at work. If symptoms begin to interfere with everyday activities, a Multiple Sclerosis Rehabilitation team can address problems with mobility, dressing and personal care, role performance at home and work, and overall fitness. They also provide evaluation and treatment of speech and swallowing difficulties and problems with thinking and memory.
When you have multiple sclerosis (MS), you may have certain physical and cognitive challenges. Multiple Sclerosis Rehabilitation-including physical therapy, occupational therapy, speech therapy, and cognitive retraining-may help reduce these disabilities.
Multiple Sclerosis Rehabilitation is an important part of health care delivery for persons with multiple sclerosis. Since the majority of people are diagnosed between the ages of 20 and 50, the challenges of MS affect those at the peak of their career and childbearing years. Although MS can affect children, it is much less common that this age group.
MS can cause significant impairment including balance and coordination problems, muscle stiffness and weakness, cognitive problems, impaired speech or vision, extreme fatigue and even paralysis. Prognosis varies but the disease can cause loss of mobility and independence. Interest in multiple sclerosis rehabilitation has increased in recent years as research has shown it can lead to substantial improvements in patients’ quality of life. Multiple Sclerosis Rehabilitation is especially helpful for MS patients because of the often progressive and unstable nature of the disease. Patients go through periods of remission and flare up, and symptoms change over time; Multiple Sclerosis Rehabilitation must be adjusted accordingly.
Multiple Sclerosis Rehabilitation is considered a necessary component of comprehensive, quality health care for people suffering with MS, at all stages of the disease.
Cause Of Multiple Sclerosis
Epidemiological studies of MS have provided hints on possible causes for the disease. Various theories try to combine the known data into possible explanations, but none has proved definitive. MS likely occurs as a result of some combination of both environmental and genetic factors.
1)Genetic factors
MS is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease. HLA region of Chromosome 6. Changes in this area increase the probability of suffering MS.
2)Infectious cause
Evidence for viruses as a cause includes the presence of oligoclonal bands in the brain and cerebrospinal fluid of most patients, the association of several viruses with human demyelinating encephalomyelitis, and induction of demyelination in animals through viral infection. Human herpesviruses are a candidate group of viruses linked to MS; Varicella zoster virus has been found at high levels in the cerebrospinal fluid of MS patients, but the most reproduced finding is the reduced risk of having the disease in those who have never been infected by the Epstein-Barr virus, together with the correlation of its markers with disease activity.
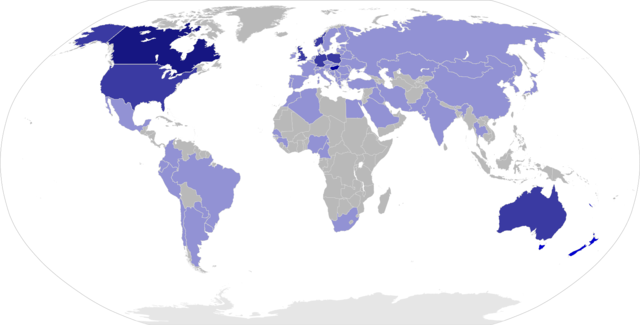
3)Non-infectious environmental risk factors
MS is more common in people who live farther from the equator. Decreased sunlight exposure has been linked with a higher risk of MS. Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun. Severe stress may also be a risk factor although evidence is weak; Smoking has also been shown to be an independent risk factor for developing MS. Association with occupational exposures and toxins—mainly solvents—has been evaluated, but no clear conclusions have been reached. Vaccinations were also considered as causal factors for the disease; however, most studies show no association between MS and vaccines. Several other possible risk factors, such as diet and hormone intake, have been investigated; however, more evidence is needed to confirm or refute their relation with the disease.
Definitions and Terminology Used to Describe Categories of Multiple Sclerosis
- Relapsing-remitting multiple sclerosis (RRMS);Characterized by relapses with either full recovery or some remaining neurological signs/symptoms and residual deficits upon recovery; the period between relapses are characterized by lack of disease progression.
- Primary-progressive multiple sclerosis (PPMS);Characterized by disease progression from onset, without plateaus or remissions or with occasional plateaus and temporary minor improvements.
- Secondary-progressive multiple sclerosis (SPMS);Characterized by initial relapsing-remitting course, followed by progression at a variable rate that may also include occasional relapse and minor remissions.
- Progressive-relapsing multiple sclerosis (PRMS);Characterized by progressive disease from onset but without clear acute relapses that may or may not have some recovery or remissions; commonly seen in people who develop the disease after 40 years of age.
- Benign multiple sclerosis; Characterized by mild disease in which patients remain fully functional in all neurological systems 15 years after disease onset.
- Malignant multiple sclerosis (Marburg's varient); Characterized by rapid progression leading to significant disability or death within a short time after onset.
Multiple Sclerosis Pain
Some of the most common types of pain experienced by multiple sclerosis patients include:
Acute Multiple Sclerosis pain.
These come on suddenly and may go away suddenly. They are often intense but can be brief in duration. The description of these acute pain syndromes are sometimes referred to as burning, tingling, shooting, or stabbing.
Trigeminal neuralgia or "tic doloureux."
A stabbing pain in the face that can be brought on by almost any facial movement, such as chewing, yawning, sneezing, or washing your face. People with MS typically confuse it with dental pain. Most people can get sudden attacks of pain that can be triggered by touch, chewing, or even brushing the teeth.
Lhermitte's sign. A brief, stabbing, electric-shock-like sensation that runs from the back of the head down the spine, brought on by bending the neck forward.
Burning, aching, or "girdling" around the body. This is called dysesthesia by physicians.
There are also some types of pain related to MS that are described as being chronic in nature -- lasting for more than a month -- including pain from spasticity that can lead to muscle cramps, tight and aching joints, and back or musculoskeletal pain. These chronic pain syndromes can often be relieved by Multiple Sclerosis Rehabilitation- anti-inflammatory drugs, massage, and physical therapy.
Multiple Sclerosis Alternative Treatment
Medications and physical therapies can be complemented by alternative treatment. See your health care provider for information, advice and possible referral. The range of alternative treatments in Multiple Sclerosis Rehabilitation that may be helpful include:
- Acupuncture
- Biofeedback therapy
- Chiropractic
- Hypnosis
- Massage
- Meditation
- Relaxation techniques
- Tai chi
- Yoga
Multiple Sclerosis Prognosis
Only a small percent of patients actually die as a consequence of the disease. For most individuals, life expectancy is not reduced, with 74 percent of patients surviving 25 years after onset of symptoms. However only a minority of individuals with MS are still in the workforce 10 years after onset. At 15 years, 50 percent of patients will require the use of an assistive device to walk, and at 20 years, 50 percent of patients will require a wheelchair. Despite its variable course, certain prognostic factors have been identified in MS.
Symptoms; Onset with only one symptom is one of the strongest indicators of a favourable prognosis.
Course of disease; Benign and RRMS are associated with a more favourable prognosis whereas PPMS is generally considered more ominous.
Age; Young age at onset is more favourable than onset after age 40, which is associated with a PPMS course and increased disability.
Neurological findings at 5 years are one of the most important prognostic factors; significant pyramidal and cerebellar signs with involvement at multiple sites at 5 years is associated with a poor prognosis and more severe disability.
MRI findings; Favourable prognostic factors include low total lesion burden, low active lesion formation, and negligible myelin and axon loss.
It is important to remember that these remain general guidelines and cannot be used to describe outcomes for individual patients.
Types of Multiple Sclerosis Rehabilitation Therapies are
- Physical Therapy (PT) in Multiple Sclerosis Rehabilitation The physical therapist evaluates and addresses the body’s ability to move and function, with particular emphasis on walking, strength, balance, posture, fatigue, and pain. PT might include stretching, range-of-motion and strengthening exercises, gait training, and training in the use of mobility aids (canes, crutches, scooters and wheelchairs) and other assistive devices. The ultimate goal is to achieve and maintain optimal functioning and prevent unnecessary complications such as de-conditioning, muscle weakness from lack of mobility, and muscle contractures related to spasticity.
- Occupational Therapy (OT) in Multiple Sclerosis Rehabilitation The goal of OT is to enhance independence, productivity, and safety in all activities related to personal care, employment, and leisure activities. Occupational therapists provide training in energy conservation techniques and the use of adaptive tools and devices to simplify tasks at home and in the office. They recommend strategic modifications to the home and workplace to ensure accessibility and convenience. Occupational therapists also evaluate and treat problems with thinking and memory.
- Therapy for Speech and Swallowing Problems in Multiple Sclerosis Rehabilitation The speech/language pathologist (SLP) evaluates and treats problems with speech and/or swallowing—both of which can result from damage in the CNS that reduces control of the muscles used in these important functions. The goal of therapy is to enhance ease and clarity of communication and promote safe swallowing and overall health. Some SLPs also evaluate and treat problems with thinking and memory.
- Cognitive Rehabilitation Neuropsychologists, as well as many occupational therapists and speech/language pathologists, evaluate and treat changes in a person’s ability to think, reason, concentrate or remember. While these professionals use different evaluation and treatment strategies, they share the common goal of helping people function optimally if cognitive changes are experienced.
- Vocational Rehabilitation State vocational rehab programs offer job readiness training, job coaching, job placement assistance, mobility training, and assistive technology assessments—with the goal of helping people maintain their current employment or find new employment that accommodates their needs.
Physical Therapy Role in Multiple Sclerosis Rehabilitation
Unlike most other neurological disorders, including spinal cord injury, traumatic brain injury, and stroke, there is no “fixed deficit” in MS; symptom profile, lesion burden on MRI, and disease course vary over time. Therapists must be prepared to treat each MS patient individually, and with flexibility, over the long term. In Multiple Sclerosis Rehabilitation, there are no protocols or time limits—just a unique opportunity to employ numerous problem-solving skills, interventions, and resources. And because MS affects not just an individual, but a whole family, it is a disease that benefits from a team approach as in Multiple Sclerosis Rehabilitation— making coordination and communication with other health care providers extremely important.
Clinical Challenges in Multiple Sclerosis Rehabilitation
MS poses a variety of clinical challenges that can impact Multiple Sclerosis Rehabilitation interventions: For example, thevery common symptoms of weakness and fatigue caused by impaired nerve conduction in the central nervous system, can be exacerbated by a variety of factors:
- An elevated core body temperature (from overheating, overexertion, or infection with fever)
- Certain medications, such as those used to treat spasticity and pain
- Obesity
- Disrupted sleep (caused by bladder urgency, periodic limb movements, spasticity, and pain, among other factors)
- Affective disorders such as depression
- Stress
- Other medical conditions, such as anemia
Many other “invisible” symptoms are cause for frustration in patients, including impairments of sensation, vision, cognition, bowel and bladder, and sexual function—all of which need to be acknowledged and addressed by the rehabilitation specialist.
Interventions throughout the Disease Course by Multiple Sclerosis Rehabilitation-
At the Time of Diagnosis
Patients newly diagnosed with MS benefit from education, support and a baseline evaluation by an experienced PT. At this time, misunderstandings about the disease and its management, the importance of appropriate exercise/activity, fatigue issues, and any subtle gait or balance impairments can be addressed. Follow up should be on an “as needed” basis by Multiple Sclerosis Rehabilitation.
Following Acute Exacerbations
Physical therapy following an acute exacerbation (also called a relapse or attack) should have the goal of carefully helping the person return to baseline functioning. It is customary to wait two weeks after the attack before starting or resuming outpatient PT, because of weakness, lack of sleep from IV steroids, or other factors.
Progressive Disease
Patients with primary-progressive MS do not have remissions; their functioning declines gradually, but steadily, over time. Patients who transition from relapsing-remitting MS to secondary-progressive MS are not able to return to baseline (due to progression of the disease that occurs between exacerbations) and demonstrate a slow decline in function. Because both groups have a huge emotional burden in addition to their physical challenges, physicians are encouraged to refer a person proactively to PT rather than waiting until he or she is struggling. Focus should be on support, resourcing, avoiding de-conditioning, maintaining safety, and maximizing health andindependent function. Assessment of the need for mobility aids now and in the future is essential for these patients, and it is especially beneficial for the PT to assist the physician in assuring that the appropriate detailed prescription or letter of medical necessity (LOMN) is provided.
Advanced MS
Patients in advanced stages of MS have significant disease burden, are non-ambulatory, and at risk for other secondary health conditions. Physical therapy for this population will likely be focused on seated trunk positioning and control, transfers, upper extremity strength, respiratory function, andequipment needs. The use of standing devices or standing wheelchairs can be very helpful, providing weight bearing on the long bones, stretching to ease spasticity, relief for bowel and bladder, and improved respiration and speech projection.
Physical Therapy Assessment
At the initial session, taking a thorough history is critical. The history should include date of diagnosis, date and nature of initial symptom(s), other health conditions, medications, prior level of activity, and “top three problems” in the order that they interfere with quality of life. This prioritization will guide the Multiple Sclerosis Rehabilitation goal-setting.
The PT evaluation in Multiple Sclerosis Rehabilitation should be structured to respect fatigue, but provide a good overview of thepatient’s baseline. Some standardized testing might be spread out over several follow-up sessions of Multiple Sclerosis Rehabilitation to avoid patient burn-out and frustration. If a patient’s primary problem is “wobbly walking”, for example, a gait assessment should be performed both at the beginning and the end of the initialsession to determine impact of fatigue on weakness and balance. It is also very important to have a variety of trial ambulation aids in the clinic—to introduce them to the patient (initial reluctance to accept an aid is common) and to determine “best fit” for the Multiple Sclerosis Rehabilitation.
The use of some standardized assessment tools in the assessment process is recommended;however few of those tests routinely used in PT have been evaluated specifically for the MS population. The few measures currently standardized for MS are:
- MS Functional Composite (MSFC), which includes the 25-foot walk
- Expanded Disability Status Scale (EDSS)—performed by trained physicians and nurse practitioners
- MS Fatigue Impact Scale (MSFIS)
- Disease Steps (DS)
- MS Walking Scale-12 (MSWS-12), a patient self-report
Other tests that are useful include:
- Berg Balance Scale
- Tinetti Gait and Balance Assessment
- Activities Specific Balance Confidence (ABC)
- Timed Up and Go (TUG)
- Dynamic Gait Index (DGI)
- Functional Independence Measure (FIM)
- 2-minute walk, 6-minute walk
- Borg’s Rate of Perceived Exertion
The PT evaluation can include a broad overview, so it’s important to prioritize time spent, with the patient’s primary issues addressed first.
- Posture, Trunk Control, Balance, Transfers It is important to assess seated and standing posture and static and dynamic balance. Balance impairments are common in MS, increasing the risk of falls. When appropriate, transfers to and from bed, chair, toilet, car and floor should be evaluated—noting quality, safety, and level of assistance needed. Begin a fall risk/safety profile to guide treatment planning in Multiple Sclerosis Rehabilitation. A PT can provide balance retraining through exercises that emphasize strengthening and flexibility. Balance can be improved through use of visual cues or techniques to reduce upper-extremity tremors. Relaxation training is often used as therapy.
- Ambulation/Mobility
Since walking requires balance, coordination, upper body control, strength, and endurance, rehab for walking requires evaluation of all of these areas. The tools for mobility are now lighter, easier to handle, more attractive, and more comfortable than ever. A PT can determine which mobility tools are appropriate to your needs and teach you the skills you need to use them well.
For the ambulatory individual, the desire to continue walking or “to walk better” is usually a primary goal. Vision, sensation, vestibular or cerebellar deficits, spasticity, muscle weakness, fatigue and shoe wear need to be considered in addition to posture and balance for Multiple Sclerosis Rehabilitation. The most appropriate ambulation aid(s) should “normalize” the gait pattern with improved alignment, stability, control and confidence and a decrease in energy expenditure. A person’s needs often vary with level of fatigue, temperature, distance to be walked or time of day. Popular options in Multiple Sclerosis Rehabilitation are folding canes (with palm grip handles), lightweight forearm crutches, and four-wheeled rolling walkers (with large swivel wheels for easier maneuvering outdoors and on carpets, a flip-up seat without a front cross bar for more erect posture when walking and the opportunity to sit and rest when needed, a flexible backrest, and user-friendly hand-brakes). Other effective ambulatory aids for patients with foot drop include custom ankle-foot-orthoses (AFOs) made of lightweight plastics—articulated or solid—or the newer ultra lightweight carbon composite materials, hip-flexion-assist-orthoses (HFAO), or the new wireless functional electrical stimulators (FES).The Lokomat does more than move the legs. Feedback is provided on the screen for reinforcement.
- Range of Motion (ROM) Both passive and active functional ROM should be assessed in the extremities and trunk, limiting detailed goniometric measurement to noted problem areas for time and fatigue reasons. Sedentary or inactive persons with MS often present with significant tightness in hip flexors, adductors, hamstrings and heel cords. Limited overhead reach is often noted in those with slumped posture due to tightness in the pectoralis minor, major and latissimus dorsi. Poor head control due to postural and substitution patterns often leads to tightness in the upper trapezius and posterolateral cervical muscles.
- Motor Function Assessment should focus on gross strength, with emphasis on function, in the extremities and trunk. Focus specific muscle testing on problem areas to minimize fatigue. Quality and control of movements, as well as substitution patterns, need to be noted for Multiple Sclerosis Rehabilitation. A key is to prevent or correct “secondary” or “disuse” weakness, commonly seen in persons with MS who have assumed a sedentary lifestyle or embraced compensatory movement patterns. Weakness due to inactivity and poor posture is frequently found in the trunk, lower abdominals, gluteus medius and maximus, middle and lower trapezius, and high anterior neck flexors. Muscle imbalances of anterior/posterior tightness versus weakness (such as the iliopsoas and gluteus maximus) frequently respond favorably to a corrective exercise program and postural correction and awareness.
- Neurological Function Assessment of neurological symptoms is necessary in Multiple Sclerosis Rehabilitation for development of treatment interventions (to supplement pharmacologic therapies) for improved safety, control and function. Common problems include abnormal tone—usually hyper-tonicity (which may be constant, fluctuating, or intermittent)—clonus, and tremors (can be “resting”, “intention” or both). Note interference with function. Other deficits relate to coordination, sensation (hyper or hypo), proprioception and pain. Referral to a neurologist, physiatrist, or pain specialist for additional treatment interventions may be warranted in Multiple Sclerosis Rehabilitation.
Normal movements require a coordinated sequence: As one muscle contracts, an opposing muscle must relax. MS can disrupt this process, resulting in the simultaneous contraction of opposing muscles. Th is is called spasticity. The affected body part becomes stiff or difficult to move and tends to feel very tight. Spastic sensations may range from neutral to mildly unpleasant to very painful. In severe cases, spasticity can even cause a limb to become “frozen” in a bent position, requiring immediate medical attention.
Spasticity can be managed in Multiple Sclerosis Rehabilitation with the help of a physician and a PT. A combination of medication, exercises, adaptive devices, and relaxation techniques may be prescribed. Exercise programs will likely include stretching and range-of-motion exercises. Exercise in acool swimming pool is helpful because the buoyancy of the water makes smooth movements easier. Passive exercise (when someone else moves your body) is particularly effective for managing spasticity. Specific positioning can also help to decrease spasticity.
- Physical fitness Appropriately designed exercise programs in Multiple Sclerosis Rehabilitation are of enormous benefit to people with MS. Exercise helps maintain or even build endurance. After a flare-up of MS symptoms, exercise can help restore function and re-energize a person. A PT, physiatrist, or exercise physiologist in Multiple Sclerosis Rehabilitation can provide the best advice on a good program that includes aerobic and non-aerobic exercises. It is best to seek help from someone familiar with MS.
- Pain from awkward positionsThe medical term is “musculoskeletal dysfunction.” It results from unusual positioning of the body caused by MS symptoms. For example, hip, knee, or low back pain can stem from an odd standing position that a person has developed in an attempt to maintain balance. Fatigue can make this kind of pain even worse. Overuse of certain muscles to compensate for other muscles canalso lead to pain. A physician will need to determine whether your pain is caused by nerve damage or by musculoskeletaldysfunction in Multiple Sclerosis Rehabilitation. If the latter has occurred, a PT can devise a program of strengthening and stretching exercises, practice of proper positioning, and compensatory techniques, such as bracing or use of an assistive device, to prevent awkward or excessive use of joints or muscles.
- Pressure sores Many changes in the body may occur if mobility is severely impaired. A person who is immobile runs the risk of developing pressure sores. These occur when the skin breaks down from constant pressure caused by sitting or lying in one position. This pressure cuts off the blood supply to the underlying skin, fat, and muscle. These sores usually occur over bony prominences such as the tailbone, buttock, heel, shoulder blade, elbow, and possibly the back of the head. Sores may also develop from friction to the skin. This is called shear and may result from sliding across a bed or wheelchair. The skin is much more likelyto break down if it is moist or infected. Thus incontinence(not being able to control urine or bowel movements, or both) can add to the problem.The best way to treat a pressure sore in Multiple Sclerosis Rehabilitation is to avoid developing one in the first place. Pressure sores can be prevented in the following ways: Get up or change positions frequently, or have someone assist you to change your position at least every two hours. Keep the skin clean and dry. Check skin for reddened areas or sores during self-care routines. And make sure nutrition and fluid intake is adequate. The treatment of pressure sores in Multiple Sclerosis Rehabilitation becomes more difficult as the sore advances. It is imperative to see your physician if you suspect that a pressure sore has begun.
- Respiratory Function It is important to recognize that respiratory problems are common in more disabled patients, but also exist in a large number of persons with MS that have minimal disability. Some people find that relaxation techniques and deep breathing, such as those used in yoga or t'ai chi, for example, help them relax when exercising. These kind of techniques can be learned with books or tapes, or through classes. If you join a class, you might want to explain your needs to the teacher beforehand so that they are aware of any adjustments you might want. It is important to take any exercise at a pace that suits you.
- Wheeled Mobility The use of a wheelchair or scooter is often appropriate when long distances must be covered and energy conservation is required, allowing needed community access. Some persons with MS prefer a standard wheelchair because of its portability, but adequate upper body strength and endurance are needed. In most cases, motorized wheeled mobility is the better choice for long term independence. A scooter (or “power operated vehicle”) is useful for individuals in Multiple Sclerosis Rehabilitation with significant fatigue, weakness, paraparesis or ataxia who retain good dynamic sitting balance and transfer skills. A power wheelchair would be more appropriate for individuals who are minimally or non-ambulatory and require additional seat and trunk support. In all cases Multiple Sclerosis Rehabilitation, consideration must be given to vision, cognition, safety awareness, and access to home and vehicle.
- Other Important Considerations Persons with MS have many other issues that need to be considered in Multiple Sclerosis Rehabilitation as part of the PT evaluation, goal-setting and when making referrals to other team members. In addition to vision, cognition and speech or swallowing problems, it’s important to consider each patient’s support/social network, emotional stability (depression is common), and vocational/homemaking history in Multiple Sclerosis Rehabilitation.
Goal Setting and Treatment Plans
It is essential in Multiple Sclerosis Rehabilitation that the short-term therapy goals be patient driven (their “wish list”), functionally focused, realistic and attainable. Each PT should attempt to teach corrective exercises and activities that can easily be followed in the home or community to supplement any clinic equipment that might be used. Some “food for thought”: If leg weakness, fatigue, and impaired gait are primary issues, the patient will benefit more from functional activities done in(supported) standing than s/he will from 3 sets of 10 leg lifts or 20 minutes on a stationary bicycle. There is a lot to be said for specificity of training in Multiple Sclerosis Rehabilitation with this population. In every case, fatigue must be respected, overheating avoided, and rest intervals provided—excellentopportunities for education and resourcing (which should be billed as “therapeutic activities”) during the treatment session. Long-term goals in Multiple Sclerosis Rehabilitation should include an effective home and community program with less dependence on formal physical therapy.
Home Physical Therapy Programs
The key components of a successful home program are that it is enjoyable, varied, goal-oriented and realistic. Compliance issues include fatigue, poor motivation, depression, lack of needed support or assistance from family and friends, time constraints, and cognitive dysfunction (usually short-term memory, attentional, or sequencing deficits, which requires the therapist to provide the exercises in written instructions and pictures). Emphasis needs to be placed on corrective exercises to: (1) improve function (restoring alignment, mobility, and strength/endurance lost due to inactivity/disuse or compensatory movement patterns), (2) manage spasticity (slow stretching, cold packs, controlled position changes), and (3) control energy management (careful pacing, flexible work and activity schedules, pro-active resting vs. reactive “collapse”, avoiding overexertion/ overheating, and substitution of less stressful /strenuous/frustrating activities). Compliance is enhanced if the patient notes slow steady progress toward reaching the goals of improved symptom management and increased activity and participation both at home and in the community.
Managing heat during exercise in Multiple Sclerosis Rehabilitation
Not everyone with MS is affected by heat, but some are particularly sensitive. Hot weather, an over-heated room and exercise can all make MS symptoms worse. This is a temporary effect – when the body cools down again, symptoms return to the level they were before. If you are sensitive to heat, keeping cool during or shortly before exercise may help you exercise for longer, or more strenuously, without bringing on heat-related symptoms. This could be done with ice drinks, cooling garments, or with regular breaks to prevent overheating.
Research showing benefits for these cooling techniques is not conclusive, and they may not help everyone, but they are unlikely to be harmful. With the support of a health professional, you may find a cooling method that works for you. Lowering the body’s temperature, with cold baths or cooling garments, might also reduce some people’s muscle stiffness temporarily. Applying cold packs or cold towels directly to affected muscles may give temporary relief for spasms or stiffness. Again, research is not conclusive, but you may find such cooling techniques help your symptoms.
In contrast, some people with MS find that cool temperatures make their spasms or stiffness worse. For these people, exercising in a warm swimming pool may help with stretching and relaxing muscles.Be careful with hot and cold therapies. When applying cold directly to the skin, or when using cooling garments or cold water to cool the body, care should be taken not to damage the skin. MS can cause changes to the way you experience temperature, distorting the feeling that would normally tell you when something is too hot or too cold. It is sensible to consult your doctor, MS nurse or physiotherapist if you are thinking of using such techniques.
Only a physiotherapist can instruct you on the proper way to exercise in Multiple Sclerosis Rehabilitation.
Follow-up
Optimal follow-up for outpatient therapy will vary according to individual needs, and typically varies from the “traditional” (orthopedic or fixed deficit neurological condition) model of 2–3 times/week for 6–8 weeks. Dedicated one-on-one sessions should be scheduled “as needed” since the need for Multiple Sclerosis Rehabilitation is life long and likely to increase with age. Consideration must be given to the numerouscompliance challenges, including transportation, weather (cold causes stiffness, high heat and humidity cause weakness), and lack of energy, motivation or support. Continuity with therapyprovider(s) is another important consideration for improved compliance with follow-up. Initially it might be appropriate for patients to be scheduled 1–2 times a week to meet short-term goals. Then the frequency should lessen to weekly or every other week until symptoms are controlled and an effective home/ community Multiple Sclerosis Rehabilitation program has been established. At that time follow-up should be “prn” to revise or augment the program or trouble-shoot any new problems.
Occupational Therapists (OTs) Role in Multiple Sclerosis Rehabilitation
Occupational Therapists (OTs) focus on skills that require upper-body strength, coordination, and fine-motor control. These include all the “occupations” of daily life, such as bathing, toileting, household chores, and working at a job. OTs also focus on cognitive problems, and can assist with cognitive retraining and strategies to compensate for poor memory. Most important, OTs can help with energy conservation.
- multiple sclerosis fatigue Fatigue is one of the most common symptoms of MS, and sometimes the most disabling one. It affects everything you do.Your physician may prescribe medications and regular rest periods. Fatigue is also managed by conserving energy and working efficiently. OTs are the experts on labor saving and energy-conservation techniques. Ask your physician for a referral if fatigue is disrupting your life.
- Upper body function An OT can recommend exercises to improve the strength and coordination of your arms and hands. Doing so can improve independence and function in your daily activities.
- Driving Driving can be affected by many MS-related disabilities. An OT can assess your driving skills and determine whether the available adaptations will work for you. Testing should be conducted both in the OT’s office and on the road. Bear in mind that the laws regarding what kinds of testing and reporting are necessary vary from state to state.Hand controls for braking and acceleration are available for people who cannot rely on their legs. Steering knobs can help people who have the use of only one arm. And wheelchair lifts can be installed in certain cars and vans for drivers and passengers who use scooters or wheelchairs
- Computers and electronic equipment Computers open a world of recreation and job-related activities, but MS symptoms may require special adaptations. For example, people with vision problems can use computers with enlarged keyboards, magnifying displays, or text-to-speech programs that read aloud the material onscreen.Electronic remote controls can be used for virtually all the appliances in an environment—lights, radios, telephones,televisions, air conditioners, even doors. An OT can help you determine which devices are most appropriate, and where you can get any training that’s needed.
- Daily occupations The “occupations” of occupational therapy include the everyday things you do—caring for yourself and your household, holding a job, recreation. Bathing, toileting, dressing, eating, and household chores may become hard to do in the presence of certain impairments. An OT can advise you about techniques and adaptive devices to compensate for particular disabilities.
Vocational Rehabilitation Specialist's Role in Multiple Sclerosis Rehabilitation
Vocational Rehabilitation Specialists focus on retraining or use of adaptations and accommodations on the job. They may work independently or in consultation with your OT.
Psychologist's Role in Multiple Sclerosis Rehabilitation
Psychologists help people learn ways to handle their emotional and cognitive problems and deal with the impact of MS on the family.
Sexuality
Neurologists, urologists, sex therapists, specialized nurses, and psychologists may all play a role in addressing sexual problems caused by MS. Men may have difficulty achieving or maintaining erections, or reaching orgasm; women may experience impaired sensation, numbness or tingling in the genital area, insufficient lubrication, or difficulty reaching orgasm.
MS also affects sexual responses indirectly. Fatigue, pain,bowel or bladder problems, and the emotional impact of having MS can dampen sexual desire. Spasticity may prevent using certain positions.
Taking an active approach to sexual problems means that both partners explore adaptations in sexual expression. If you find these conversations difficult, a psychologist can help start this process. Medical treatment to manage symptoms is part of the solution. So is attention to the emotional concerns of both partners.
Neuropsychologist's Role in Multiple Sclerosis Rehabilitation
Neuropsychologists specialize in memory, problem solving, and other cognitive problems, and can assess individuals for the most precise diagnosis of these difficulties.
Memory loss and other cognitive difficulties Poor recent memory is the most commonly reported cognitive symptom in MS. Psychologists, speech pathologists, and OTs can recommend teach simple compensatory strategies, such as making lists, writingnotes, learning memory tricks, and keeping a “memory” notebook.
People with MS can also experience problems with concentration, reasoning,judgment, and the ability to learn.A neuropsychologist may be recommended for evaluation and design of the best therapy.Restructuring daily activities and providing supervision may be needed in rare situations.
Even very mild cognitive problems can increase fear, anxiety, and depression—emotions that in themselves are disabling. A psychologist can provide supportive counseling.
Speech/Language Therapist's (or Speech/Language Pathologist's) Role in Multiple Sclerosis Rehabilitation
Speech/Language Therapists (or Speech/Language Pathologists) work with speech when MS makes talking difficult or causes swallowing problems. They can also help with problems in cognitive functioning, memory problems, and using language,which may stem from MS-related injury in the “thinking” part of the brain.
If it’s hard to speak or swallow, When MS affects parts of the brain that control muscles in the mouth, throat, or voice box, speech and/or swallowing difficulties may result. To improve speech, the therapist may teach breath control techniques or how to speak more slowly with emphasis on key words. Voice amplifiers can help when a person cannot generate volume. If speech is severely impaired, other communication devices are available. Swallowing problems may be helped by exercises,altering mealtime routines to promote relaxation, or by making changes in the diet, or the position of the body while eating.
If the words are wrong
Common language symptoms involve not being able to find the right word or using an inappropriate substitute word. These problems can be handled with compensatory techniques.
Urologist's Role in Multiple Sclerosis Rehabilitation
Urologists treat urinary infections, bladder problems, and sexual problems.
Bladder problems
Many people with MS experience bladder problems at one time or another. The most common problems are increased frequency or urgency, leakage, difficulty urinating despite having the urge to do so, and the inability to hold urine in the bladder. Sometimes the bladder does not empty completely, which can set the stage for urinary tract infections. Diagnosis is the first step. Symptoms may then be managed by medications, diet changes, and in some cases self-catheterization, in which a small tube, or catheter, is inserted through the urethra into the bladder so urine can drain out. (This sounds difficult and painful, but mostpeople can learn to do it easily and comfortably.) There are also exercises involving the pelvic floor muscles that may be appropriate.
Gastroenterologist's Role in Multiple Sclerosis Rehabilitation
Gastroenterologists focus on serious bowel difficulties.
Bowel problems
Constipation may occur because of MS-related neurologicaldamage,or lack of exercise,inadequate fluids,or poor diet. The first line of therapy usually involves modifying the diet to include more fruits,vegetables,and whole grains,and six to eight glasses of water each day.If these measures don’t solve the problem,consult your physician or nurse.A gastroenterologist will be needed in difficult situations.
Incontinence, or loss of bowel control, is a much less frequent complication and may result from leakage around impacted stool. Stool bulkers, a regular “bowel program,” and medication may also be prescribed. A physiatrist may also be very helpful with both bowel and bladder problems.
Nurse's Role in Multiple Sclerosis Rehabilitation
Nurses— First and Last.
A nurse can be the linchpin of your rehab program. Nurses are trained to identify health problems, do assessments, and connect people to appropriate specialists. “Patient education” is on their job description and nurses will make time to listen to your questions and teach you self-help techniques.
Living with MS
Living well with MS means much more than getting treatment for symptoms, adopting new techniques, and adjusting to physical changes. It means accepting MS as part of your life. Accepting without giving in is not an easy task, and there is no one right way to do it.
Multiple Sclerosis Rehabilitation provides some of the tools you need to take control of your MS rather than having MS take control of you. Counseling by a psychologist, social worker, or psychiatrist who has worked with people who have chronic diseases may be extremely helpful.
It may also be helpful to meet other people who live with MS. Support groups, self-help meetings, and trained peers with MS all provide a chance to share information and concerns.
References
- NCBI MS
- Houtchens MK, Lublin FD, Miller AE, Khoury SJ. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Daroff RB, Fenichel GM, Jankovic J, Mazziotta JC, eds. Bradley’s Neurology in Clinical Practice. 6th ed. Philadelphia, Pa: Elsevier Saunders; 2012:chap 54.
- Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302
- Multiple Sclerosis- Wikipedia
What Other Visitors Have Said
Click below to see contributions from other visitors to this page...
Bee Therapy (apitherapy) for MS Not rated yet
Bee sting therapy is a type of “apitherapy,” a term which refers to the use of bee products to treat medical conditions. Other forms of apitherapy include …
Return from multiple sclerosis rehabilitation to Neuro Rehab
Return from multiple sclerosis rehabilitation to Home Page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |


