Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Chronic Achilles Tendonitis
What is Chronic Achilles Tendonitis?
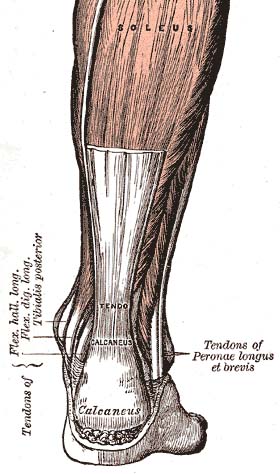
Chronic Achilles tendonitis, also sometimes called Achilles tendinitis , is a painful and often debilitating inflammation of the large tendon in the back of the ankle (achilles tendon). It is a common overuse injury that tends to occur in middle-age recreational athletes. The overuse causes inflammation that can lead to pain and swelling. Furthermore, it can lead to small tears within the tendon, and make it susceptible to rupture.
Achilles Tendon Dysfunction
The Achilles tendon is the largest and strongest tendon in the body. The tendon has no true synovial sheath but is encased in a paratenon of varying thickness. The vascular supply to the tendon comes distally from intraosseous vessels from the calcaneus and proximally from intramuscular branches. There is relative area of avascularity 2-6 cm from the calcaneal insertion that is more vulnerable to degeneration and injury. Achilles tendon injuries are commonly associated with repetitive impact loading due to running and jumping. The primary factors resulting in damage of the Achilles tendon are training errors such as sudden increase in activity, a sudden increase in training intensity (distance, frequency), resuming training after a long period of inactivity, and running on uneven or loose terrain . Achilles dysfunction can also be related to postural problem (e.g., pronation), poor footwear (generally poor hindfoot support), and a tight gastrosoleus complex.
Causes of Chronic Achilles Tendonitis
There may be several factors leading to Chronic Achilles Tendonitis:
- Overuse of the Achilles tendon
- Tight calf muscles
- Lots of uphill running
- Increasing the amount or intensity of sports training, sometimes along with switching to racing flats, which are racing shoes with less heel lift
- Over-pronation, a problem where your feet roll inward and flatten out more than normal when you walk or run
- Wearing high heels at work and then switching to lower-heeled shoes for exercise
- An Achilles tendon may tear when you move swiftly and forcefully. For example, the tendon might tear when you jump or start sprinting.
There are three stages of tendon inflammation:
- Peritenonitis
- Tendinosis
- Peritenonitis with tendinosis
Peritenonitis is characterized by localized pain during or following activity. As this condition progresses, pain often develops earlier on during activity, with decreased activity, or while at rest.
Tendinosis is a degenerative condition that usually does not produce symptoms (i.e., is asymptomatic). It may cause swelling or a hard knot of tissue (nodule) on the back of the leg.
Peritenonitis with tendinosis results in pain and swelling with activity. As this condition progresses, partial or complete tendon rupture may occur.
Symptoms of Chronic Achilles Tendonitis
The main complaint is pain over the back of the heel. This is 2-6 cm above the point where the tendon inserts on the heel bone. Patients with Chronic Achilles tendonitis usually experience the most significant pain after periods of inactivity. Therefore patients tend to experience pain after first walking in the morning and when getting up after sitting for long periods of time. Patients will also experience pain while participating in activities, such as when running or jumping. Chronic Achilles tendinitis pain associated with exercise is most significant when pushing off or jumping. It may cause swelling over the Achilles tendon. Patient complains of pain when rising up on toes and pain when stretching the tendon. The range of motion of ankle may be limited.
Diagnosis
In diagnosing Chronic Achilles Tendonitis, examine the patient’s foot and ankle and evaluate the range of motion and condition of the tendon. The extent of the condition can be further assessed with x-rays, ultrasound or MRI.
Differential Diagnosis of Chronic Achilles Tendonitis
- Partial rupture of Achilles tendon
- Retrocalcaneal bursitis (of retrocalcaneal bursa)
- Haglund's deformity (pump bump)
- Calcaneal apophysitis
- Calcaneal exostosis
- Calcaneal stress fracture (positive squeeze test)
- Calcaneal fracture
- PTT tendinitis (medial pain)
- Plantar fasciitis (inferior heel pain)
Achilles Tendonitis Treatment
Treatment approaches for Achilles tendonitis or tendonosis are selected on the basis of how long the injury has been present and the degree of damage to the tendon.
In the early stage, when there is sudden (acute) inflammation, one or more of the following options may be recommended:
- Immobilization
- Ice
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- Physical therapy.
General guidelines for chronic Achilles tendonitis
- Correct underlying training and bio mechanical problems
- Stop rapid increase in mileage
- Stop hill running
- Correct functional overpronation and resultant vascular wringing of the tendon with a custom orthotic that usually incorporates a medial rear foot post.
- Stop interval training
- Correct improper intensity of training, duration, schedule, hard surface, poor shoewear
- Soften a hard heel counter or use shoe counter heel cushions to minimize posterior "rubbing" symptoms.
- Begin a runner's stretching program before and after exercises.
-Oral anti-inflammatories (COX-2 inhibitors).
-Avoid cortisone injections ; this will cause weakening or rupture of the tendon.
-Cryotherapy (ice massage)after exercise for anti-inflammatory effect.
-Correct leg length discrepancy if present. First try 1/4 inch heel insert for a half inch leg length discrepancy; if not improved, go to 1/2 inch insert. Overcorrection (too rapid an orthotic correction) may worsen symptoms.
-Shock wave Therapy
-If symptoms persist after 4-6 weeks of conservative measures, immobilization in a removable cam boot or cast may be required for 3-6 weeks.
-Slow, painless progression to preinjury activities
- swimming
- deep water running
- bicycling
- walking
- eccentric exercises for Achilles strengthening
- light jogging
-Eccentric strengthening of Achilles tendon should condition the tendon and make it less susceptible to overuse injuries; however these exercises are not used until the patient is assymptomatic and painless for 2-3 weeks.
- toe raises in pool
- plantar flexion against progressively harder therabands
- multiple sets of very light (20 pound) total gym or slider board exercises.
If these treatments fail to improve symptoms, surgery may be needed to remove inflamed tissue and abnormal areas of the tendon.
Prevention
The best treatment of Chronic Achilles tendonitis is prevention. Stretching the Achilles tendon before exercise, even at the start of the day, will help to maintain flexibility in the ankle joint. Problems with foot mechanics can also be treated with devices inserted into the shoes.
Further Reading
- Hakan Alfredson and J Cook. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. Apr 2007; 41(4): 211–216.
- Chronic Achilles Tendon Injury: An Overview. hss.edu
- Management of chronic Achilles tendinopathy. Drug and Therapeutics Bulletin.
- Achilles Tendonitis. About health
- McLauchlan GJ, Handoll HH. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Database Syst Rev. 2001;(2):CD000232.
- Fahlström M, Jonsson P, Lorentzon R, Alfredson H. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003 Sep;11(5):327-33.
Return from Achilles Tendonitis to sports physical therapy
Return from Chronic Achilles Tendonitis to Home page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |

