Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Myocardial Infarction Treatment
Myocardial infarction treatment attempts to save as much myocardium as possible and to prevent further complications.
What is myocardial infarction or ischaemic heart disease?
Acute myocardial infarction (AMI), commonly known as a heart attack, is the interruption of blood supply to a part of the heart, causing heart cells to die. This is most commonly due to occlusion (blockage) of a coronary artery following the rupture of a vulnerable atherosclerotic plaque, which is an unstable collection of lipids (fatty acids) and white blood cells in the wall of an artery. The resulting ischemia (restriction in blood supply) and oxygen shortage, if left untreated for a sufficient period of time, can cause damage or death of heart muscle tissue.
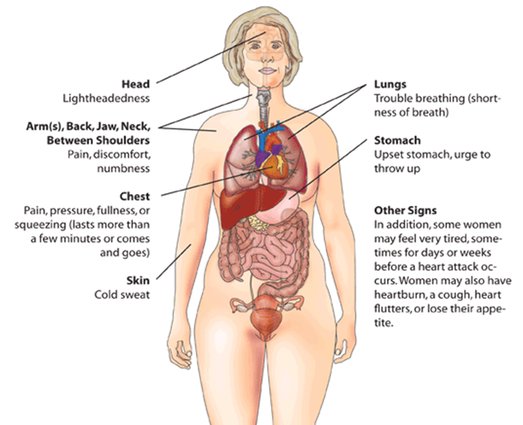
Heart attack warning signs
Myocardial infarction causes
The most frequent cause of myocardial infarction (MI) is rupture of an atherosclerotic plaque within a coronary artery with subsequent arterial spasm and thrombus formation.
Other causes include the following:
- Coronary artery vasospasm.
- Ventricular hypertrophy.
- Hypoxia due to carbon monoxide poisoning or acute pulmonary diseases.
- Coronary artery emboli, secondary to cholesterol, air, or the products of sepsis.
- Cocaine, amphetamines.
- Arteritis ,aneurysms of the coronary arteries.
- Increased afterload which increase the demand on the myocardium.
- Aortic dissection.
Symptoms of myocardial infarction
- sudden chest pain (typically radiating to the left arm or left side of the neck).
- shortness of breath.
- nausea.
- vomiting.
- palpitations.
- sweating.
- and anxiety.
Risk factors for myocardial infarction
- Diabetes (with or without insulin resistance) - the single most important risk factor for ischaemic heart disease (IHD).
- Tobacco smoking.
- Hypercholesterolemia.
- Low HDL.
- High Triglycerides.
- High blood pressure.
- Family history of ischaemic heart disease (IHD).
- Obesity.
- Age: Men acquire an independent risk factor at age 45, Women acquire an independent risk factor at age 55.
- Hyperhomocysteinemia.
- Stress.
- Alcohol Studies show that prolonged exposure to high quantities of alcohol can increase the risk of heart attack Males are more at risk than females.
Myocardial infarction treatment
Objects of early treatment
- 1). Provide cardiac resuscitation and to keep the patient alive.
- 2). Immediate hospitalization.
- 3). Treat life threatening problems.
- 4). Remove pain and suffering.
- 5). Preserve as much myocardium as possible by dissolution of Blood Clot or Thrombus, Blocking Lumen of Coronary Artery.
Myocardial infarction treatment of the early stage of attack (0- 4 hrs approx) :
In this stage patient is in severe pain, he is at risk of sudden death.
Patient's needs are:
- 1.reassurance
- 2.relief of pain
- 3.drugs to reduce pulmonary congestion
- 4.drugs to maintain circulation
- 5.monitoring rhythm
- 6.re-establishment of coronary flow
- 7.oxygen administration
- 8.if there is cardiac arrest then cardiac massage and artificial respiration.
In these cases patient and family must understand what is happening.
Myocardial infarction treatment in hospital phase (4 hrs - 9 days):
Treatment should be conducted in coronary care unit.
Treatment offers:
- 1.Treatment of arrhythmic complication.
- 2.Treatment of failure of function of pump of the heart.
- 3.Avoidance of other complications.
Arrhythmia:
In case of lethal arrhythmia, constant monitoring of the heart rhythm allows instant recognition of ventricular fibrillation and its electric conversion using direct current shock. Paddles are placed in front and back of the chest and a current is passed through the chest usually about 300 joules. This electric conversion should be followed by drugs.
Treatment of heart failure:
Treatment is difficult. Diuretics can reduce the breathlessness by lowering the filling pressure of the heart. Forward flow can be improved by drugs which make the heart beat more strongly or drugs reducing peripheral resistance.
Occasionally counter pulsation is used when a long balloon is placed in the aorta. It is inflated during diastole, increasing arterial pressure and coronary perfusion. It is deflated during systole, reducing systolic pressure and hence reducing the work of the heart.
Thrombo-embolism:
Clotting in a peripheral vein is common among patients. When it occurs in thigh or pelvic veins pulmonary embolism may occur. The risk is higher in heart failure, with extensive infarction, or in patients with varicose veins. The risk should be reduced by early mobilisation and leg exercises. Clotting over the endocardium damaged by the infarction may lead to systemic embolism. Anticoagulation may reduce this risk.
Postural hypotension, deconditioning and morale:
Bed rest reduces physical fitness and impairs the reflexes that prevent and undue fall of blood pressure when we assume the upright position. General weakness and dizziness leads to severity of heart attack. Regular exercise and altering the posture of patient help to overcome these problems and improve patient morale. Most patients able to sit up in chair and take a few steps within 24 hrs of heart attack. As the days in hospital pass, exercise increases but the patient must avoid undue tachycardia. Before discharge patient must climb stairs in hospital.
Pericarditis:
Inflammation of the lining of the heart occurs after infarction. This is painful and is reduced by the drugs.
Frozen shoulder:
Arm and shoulder movements should be encouraged occasionally.
Myocardial infarction treatment in late phase:
Patient leaving hospital should be diagnosed, prescribed by drugs and level of exercise and activities permitted at home and the expected date of returning to work should be given.
Drugs:
Beta blockers- atenolol
Digitalis, diuretics, and vaso-dilator drugs to reduce heart failure.
Warfarin anti-coagulation
Anti-arhythmic drugs
Exercise:
Regular exercise improves the exercise tolerance of patients, increases there confidence and well-being. Regular exercise classes given under supervision is useful and economical.
Surgery:
Coronary artery surgery.
Percutaneous trans luminal angioplasty.
Thoracotomy.
Social support:
It is important in these patients because support plays a important role in these patients who have less chances of survival during the administration to hospital.
Physiotherapy role in myocardial infarction treatment programme:
- 1.complete bed rest-up to 2 days.
- 2.partial bed rest-up to 4 days.
- 3.up and about-in hospital from third or fourth day for up to 2 weeks.
- 4.after discharge from hospital: 3 weeks to 12 weeks.
- 5.outpatient rehab.-3-9 months.
Complete bed rest:
- Aims of physiotherapy :
1.to prevent accumulation of secretion in the lungs. - 2.to prevent deep vein thrombosis.
- 3.to prevent pressure sores.
- 4.to teach and encourage relaxation.
- 5.to explain the purpose of an active rehabilitation programme.
Techniques used in myocardial infarction treatment programme:
1.relaxation: lying or half-lying, conscious relaxation 10 min approx. Modified physiological relaxation may be indicated. If the patient can learn to relax, the heart rate is reduced and this aids recovery by easing the load on the heart.
2.breathing exercises: bilateral basal breathing- three times. There must be no forceful breathing. This will improve oxygenation of the blood and therefore reduces the demand on the heart.
3.free active exercises: lying or half-lying
a. ankle pumps
b. foot turning in and out
c. fingers bending and stretching
d. wrists bending and stretching
4.breathing exercises: anterior basal expansion within patients normal pattern- 3 times.
5.passive movements
6.breathing exercises: posterior basal exercises- 3 times.
7.passive movements- repeat again
8.relaxation- repeat again
Partial bed rest:
The patient is up to sit for 1-2hours per day. Feeding, washing are allowed.
Aims of physiotherapy:
- 1.to maintain clear lung fields.
- 2.to increase the load on the heart such that there is hypertrophy of the myocardium.
- 3.to educate the patient to recognize signs and symptoms of excess exercise.
- 4.to begin rebuilding the patients confidence.
- 5.to train postural awareness.
- 6.to strengthen leg and trunk exercises.
Example of myocardial infarction treatment programme:
- 1.half lying: relaxation- 5 minutes.
- 2.posterior basal breathing exercises.
- 3.half lying or lying.
alternate foot pulling up and pushing down feet circling, q-drill, gluteal contractions. - 4.diaphragmatic breathing
- 5.high sitting: posture training.
- 6.half lying: lateral basal breathing.
- 7.lying: active exercises and stretching.
- 8.lying:relaxation and posture training.
- 9.crook lying should be done 3 times.
Up and about in hospital:
The patient is allowed to wash, feed, go to the toilet and have a bath-with supervision.
Aims of physiotherapy:
- 1.To continue promoting hypertrophy of the heart muscle to strengthen trunk and leg muscles.
- 2.To continue rebuilding patient confidence.
- 3.To improve exercise tolerance to teach awareness of exercise capacity.
Myocardial infarction treatment programme:
- 1.stop formal relaxation.
- 2.stop localized breathing exercises.
- 3.stride standing: holding bedrail or chair-knees and hips bending and stretching.
- 4.bend standing: elbow circling.
- 5.standing:arms raising forwards and upwards.
- 6.walk standing: one hip and knee bending forward and stretching.
- 7.standing:posture checking.
- 8.sitting:deep breathing exercises.
- 9.bend sitting: trunk bending and turning side to side.
- 10.progress each exercise.
- 11.improve confidence.
After discharge from hospital:
Home management will be given before leaving from hospital. The patient can progress the exercise a week to 10 days after discharge. Usually patient is advised not to drive car till 4-8 weeks after discharge.
Out-patient rehabilitation:
This is usually taken in gymnasium. Patients benefit from meeting fellow patients in group.
Equipment required:
- 1.defibrillator
- 2.suction apparatus
- 3.oxygen
- 4.electrocardiograph
Aims of physiotherapy:
- 1.To increase exercise tolerance.
- 2.To maintain or improve confidence.
- 3.To provide support and encouragement.
- 4.To help reduce risk factors and thereby reduce recurrence.
Myocardial infarction treatment Home Programme : General exercises
Read more about Heart Attack on Wikipedia
- 1.half yard grasp standing-one leg swinging forward and backwards then repeat with other leg.
- 2.half yard grasp standing: knees and hip bending and stretching.
- 3.yard standing: arms circling backwards.
- 4.yard standing: trunk bending and turning to touch left knee.
- 5.lying:alternate hip and knee bending and stretching.
- 6.sitting:throwing and catching ball.
- 7.standing:arms bending and stretching.
- 8.wing stride standing, trunk bending side to side.
- 9.standing:stepping up and down.
- 10.sitting ,standing up and sitting down.
- 11.stride standing: bouncing ball.
- 12.stride standing: throwing ball.
- 13.sitting:trunk turning side to side.
- 14.crook lying-pelvis raising and lowering.
Progression:
- 1.increase no. of repetitions.
- 2.increase the length of time for each exercise.
- 3.increase speed.
- 4.add weights.
- 5.alter range.
Support and encouragement is necessary in Myocardial Infarction Treatment. Golf is a suitable sport to recommend.
Content Writer- Alka Bishnoi
Return form Myocardial Infarction Treatment to Chest Physical Therapy
Return form Myocardial Infarction Treatment to Home Page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |

