Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Polio Treatment
Polio is non curable and there is no polio treatment available , bed rest during the acute stage and avoidance of injections, corrective surgery and physiotherapy along with rehabilitation helps the patient.
Physiotherapy is a cornerstone of management of polio and post polio syndrome. There is an increasing evidence base for the effectiveness of physiotherapy in alleviating PPS (post polio syndrome) associated physical problems. Patients with prior polio or post polio syndrome should have access to regular physiotherapy assessment, and treatment should be made available when needs are identified.
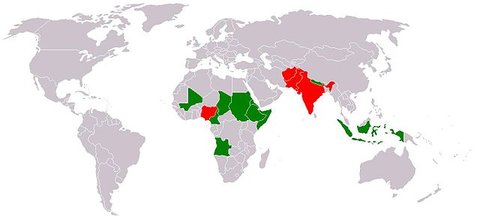
Polio worldwide 2005
Types of polio

Spinal Paralytic poliomyelitis: In this the motor neurons in the anterior horns of spinal cord are affected. Paralysis is usually asymmetrical, predominantly involves proximal muscle with pain and tenderness. Most commonly it affects the leg. Extent of weakness can vary from a single muscle group to complete tetraparesis.
Bulbar Paralytic poliomyelitis: It occurs due to damage to the medulla, pons and midbrain with dysfunction of the cranial nerve nuclei and respiratory and vasomotor regulating centres in the medulla. It can lead to respiratory muscle failure, distress of respiratory control, dysphagia, dysphonia and dysarthria. Cardiovascular, sweating and gut mobility disturbances may occur.
Bulbospinal paralytic poliomyelitis: It is also known as respiratory poliomyelitis. It has symptoms both of spinal cord and bulbar poliomyelitis. It affects the part of spinal cord C3 to C5 segments and causes paralysis of the diaphragm. Dysphagia and respiratory failure follow.
Polio encephalitis: There is inflammation of motor neurons within the brain stem, motor cortex and the spinal cord. It leads to the stiffness of back and neck, muscle cramps, headaches and paraesthesias. Paralysis occurs within 10 days after symptoms develop progress in 2 to 3 days and complete by the time fever subsides.
Polio Symptoms
There are many symptoms of polio and not everyone will experience all of the symptoms. They symptoms vary according to the type of polio the individual has. In mild polio, some of the symptoms are: headache, nausea, vomiting, general discomfort or a slight fever for up to three days. In nonparalytic polio (aseptic meningitis): the symptoms are similar to mild cases, with the addition of moderate fever, stiff neck and back, fatigue and muscle pain. The symptoms for polio and paralytic polio different. Individuals with paralytic polio experience tremor, muscle weakness, fever, stiffness, constipation, muscle pain and spasms, and difficulty swallowing.
Polio treatment
The disease may be staged as:-
Stage 1: Acute stage of paralysis: : it begins with fever and headache, followed by neck stiffness and meningitis. Muscles are painful and tender. Paralysis soon follows and reaches its maximum in 2-3 days. Limbs are weak and there may be difficulty with breathing and swallowing. If the patient does not succumb to respiratory failure, pain and pyrexia subsides after 7-10 days and the patient enters the convalescent stage.
Stage 2: Recovery/convalescent stage: : This stage is prolonged. The return of muscle power is most noticeable during the first 6 months, but there may be continuing improvement for up to 2 years.
Stage 3: Residual paralysis: : Some cases do not progress beyond the early stage of meningeal irritation. In others, however recovery is incomplete and the patient is left with some degree of asymmetric flaccid paralysis or muscle weakness.
Polio treatment in the acute stage of muscle paralysis
It involves meticulous attention to intensive care during the acute paralytic phase.
- Feeding by nasogastric tube in those with bulbar dysfunction.
- Endotracheal intubation and ventilation should be instituted in case of respiratory muscle failure or bulbar and laryngeal muscle paralysis.
- Pulmonary atelactasis and infection are treated with antibiotics and regular physiotherapy intervention.
- Rest on a firm mattress with back supported on a lumbar board. Avoid forceful exercise as this may increase paralysis. Avoid massage.
- Moist hot packs to the affected muscles produce considerable relief from the pain. Analgesics can also be used to relief pain.
- Feet to be supported by rigid boards at 90˚ angle. Early spinal bracing for the back if it is weak.
- Hip and knees should be positioned as straight as possible and arms in abduction with mild support.
- Passive range of motion for the joints to avoid contracture formation.
- Positon the patient with face down and hip extended every 2 hourly to prevent pressure sores and deformities.
Polio treatment in the recovery or convalescent stage
- Sitting up can be encouraged if the paralysis is not severe.
- As soon as the fever drops, exercises should be started to prevent contractures and return strength.
- Passive, active assisted to active resisted/ strengthening exercises, sitting balance training, standing balance training in parallel bars, gait training should be started.
- Crutches, leg braces(calipers) and other aids may help the child to move better and may prevent contractures or deformities.
- Whenever possible make exercises fun. Active games, swimming and other activities to keep limb moving as much as they can are important throughout the child’s rehabilitation.
Rehabilitation (stage 3) in poliomyelitis once all the recovery has taken place. Goals of polio treatment in the stage of residual paralysis
- Strengthening of all the innervated muscles.
- Preventing contractures and deformities.
- Making the patient as independent as possible.
- Emotional and psychological support.
Examination of the patient
A comprehensive and detailed assessment is necessary at the first consultation to establish a baseline from which future changes can be evaluated and a polio treatment plan developed. An assessment will usually have three components; neurological musculoskeletal cardiorespiratory
- neurological
- musculoskeletal
- cardiorespiratory
Neurological Examination in polio treatment include-
- New weakness in previously affected or unaffected muscles
- Decreased muscular endurance
- Gait changes
- History of falls
- Decreased function
- Other lower motor neuron signs – decreased tone, reflexes and muscle atrophy
Musculoskeletal Examination in polio treatment include-
- Range of motion testing especially for the joints affected
- Muscle testing, especially of muscles that are weak. Also test muscles that need to be strong to make up for the weak ones (shoulder strength for crutch use)
- Check for deformities, contractures, dislocations, difference in leg length, spinal curve etc
Cardiorespiratory Examination in polio treatment include-
- Reduced pulmonary function results from the virus affecting the medullary respiratory centres, the muscles of respiration and the cranial nerves.
- Thoracic cage deformity, e.g. kyphoscoliosis
- Breathing problems
- Measurement of peak flow, oxygen saturation, and interpretation of the results of pulmonary function tests
- Forced expiratory techniques such as coughing and huffing to assess a patient’s ability to expectorate secretions effectively should be assessed
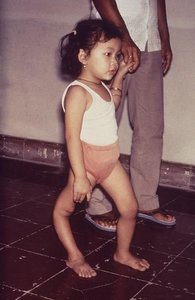
Each child will have a different combination and severity of paralyzed muscles and will have his own special needs. For some children, normal exercises and play may be all that are needed. Others may require braces or other aids to help them move about better. Those who are severely paralyzed may require wheelchair.
During the stage of residual paralysis following problems may require polio treatment.
- Isolated muscle weakness without deformity: Quadriceps paralysis may make walking impossible, it is best managed with a splint which holds the knee straight. Elsewhere, isolated weakness may be treated by tendon transfer.
- Deformity: Unbalanced paralysis may lead to deformity. At first it is passively correctable and can be counteracted by a splint. Fixed deformity require tendon transfer and joint stabilization, if necessary by arthrodesis.
- Flail joint: If the joint is unstable or flail it must be stabilized either by permanent splintage or by arthrodesis.
- Shortening: Lack of muscle activity undermines normal bone growth. Leg length inequality of upto 3 cm can be compensated for by shoe modification. Anything more may require operative lengthening of the limb.
Common biomechanical deficits in post polio
- Genu Recurvatum
- Knee flexion contracture
- Inadequate dorsiflexion in swing
- Dorsiflexion collapse in stance
- Genu valgum
- Mediolateral ankle instability
Orthotic prescription
Before prescribing orthosis it is necessary to assess:-
- Strength of hip abductors and hip extensors
- Knee extensor
- Hip, knee and ankle stability
- Strength of upper limb
- Limb length measurement and gait pattern
- Contractures and derformities
A child with foot drop can be given an ankle foot orthosis of plastic or metal. A child with weak knee may need a long-leg brace of plastic or metal. It may be with or without a knee joint that locks straight for walking and bends for sitting. Child with weak trunk may require long leg braces attached to a body brace or body jacket.
ADL’s training and occupational therapy role in polio treatment
- Washing and toilet: supporting rails, bath or shower seats and adjustments to the height of washing bowl, basin or bath may be provided
- Dressing: clothes with zip fasteners and Velcro may be provided
- Housing, domestic aids and furniture may be modified for the severely disabled
- Transport: wheelchairs must be strong enough for rough roads and be patient propelled whenever possible. Motorized wheelchairs and cars with special control are also available
Prevention
Individual children should be protected by immunization with polio vaccine. Two types of polio vaccines are available, an inactivated (killed) injectable polio vaccine (IPV) and a live attenuated (weakened) oral polio vaccine (OPV). Both vaccines are highly effective.
Prognosis
Read more about Polio on Wikipedia
During early phase of the illness, it is difficult to evaluate the extent of paralysis because of pain and spasm of the muscles. Paralyzed muscles generally recover power to a variable degree. About 5-10% of the patients may develop bulbar or respiratory paralysis. Though bulbar paralysis is not invariably fatal, many patients succumb to it. Prognosis is generally worse for the older children and in those who had a sudden onset of illness with high fever.
Return from Polio treatment to home page
Return from Polio treatment to Neuro Rehab
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |

