Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
decorticate rigidity:abnormal flexor response
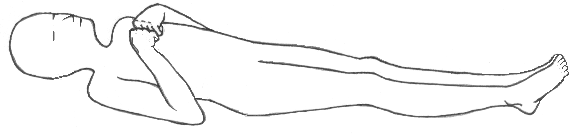
A sign of corticospinal damage, decorticate rigidity (decorticate posture, abnormal flexor response) is characterized by adduction of the arms and flexion of the elbows, with wrists and fingers flexed on the chest. The legs are extended and internally rotated, with plantar flexion of the feet. This posture may occur unilaterally or bilaterally. (See Recognising decorticate posture.)
Decorticate posture usually results from stroke or head injury. It may be elicited by noxious stimuli or may occur spontaneously. The intensity of the required stimulus, the duration of the posture, and the frequency of spontaneous episodes vary with the severity and location of cerebral injury.
Although a serious sign, decorticate posture carries a more favourable prognosis than decerebrate posture. However, if the causative disorder extends lower in the brain stem, decorticate posture may progress to decerebrate posture.
Decorticate posture
Decorticate rigidity, with arm or arms in flexion and adduction and leg(s) extended, signifies lesions at a higher level—in the cerebral white matter or internal capsule and thalamus.
ALERT If you observe decorticate posture:
- Obtain vital signs, and evaluate patient’s level of consciousness (LOC) (If LOC is impaired, insert an oropharyngeal airway, elevate his head 30 degrees, and this head to the side to prevent aspiration, unless spinal cord injury is suspected.)
- Evaluate the patient’s respiratory rate, rhythm and depth (prepare to institute emergency measures if necessary.)
- Institute seizure precautions.
- After the patient has stabilized, perform a focussed assessment.
Bilateral decorticate rigidity is essentially a bilateral spastic hemiplegia. Diagonal postures, e.g., flexion of one arm and extension of the opposite arm and leg, usually indicate a supratentorial lesion. Forceful extensor postures of the arms and weak flexor responses of the legs are probably due to lesions at about the level of the vestibular nuclei. Lesions below this level lead to flaccidity and abolition of all postures and movements. The coma is then usually profound and often progresses to brain death.
Only in the most advanced forms of intoxication and metabolic coma, as might occur with anoxic necrosis of neurons through out the entire brain, are coughing, swallowing, hiccoughing, and spontaneous respiration all abolished. Further, the tendon and plantar reflexes may give little indication of what is happening. Tendon reflexes are usually preserved until the late stages of coma due to metabolic disturbances and intoxications. In coma due to a large cerebral infarct or hemorrhage, the tendon reflexes maybe normal or only slightly reduced on the hemiplegic side and the plantar reflexes maybe absent or extensor. Plantar flexor responses, succeeding extensor responses, signify ether a return to normalcy or, in the context of deepening coma, a transition to brain death.
HISTORY
- Ask the patient about headache, dizziness, nausea, abnormal vision and numbness or tingling.
- Ask the patient’s family when decorticate posture was first noticed.
- Ask the patient’s family about behaviour changes.
RECOGNISING DECORTICATE POSTURE
Decorticate posture results from damage to one or both corticospinal tracts. With this posture, the arms are adducted and flexed. With the wrists and fingers flexed on the chest. The legs are usually extended and internally rotated, with plantar flexion of the feet.
- Review the patient’s medical history for cerebrovascular disease, cancer, meningitis, encephalitis, upper respiratory tract infection, and recent trauma.
PHYSICAL ASSESSMENT OF DECORTICATE RIGIDITY
- Take the patient’s vital signs.
- Determine the patient’s LOC, using the Glasgow Coma Scale as a reference. Be alert for signs of increased intra cranial pressure (such as bradycardia, increasing systolic blood pressure, and widening pulse pressure.) and neurological deterioration. (such as altered respiratory pattern and abnormal temperature).
- Test motor and sensory functions.
- Evaluate pupil size, equality, and response to light.
- Test cranial nerve and deep tendon reflexes.
SPECIAL CONSIDERATIONS
Assess the patient frequently to detect subtle signs of neurologic deterioration.
PATIENT COUNSELLING
Instruct the patient and his family on what to expect from diagnostic testing and treatment. Provide emotional support.
Similar pages
References
- Rapid Assessment: A Flowchart Guide to Evaluating Signs and Symptoms-By Lippincott Williams & Wilkins
- Adams & Victor's Principles of Neurology 8th 2005 McGraw-Hill
Back to home page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |



