Enhance your health with free online physiotherapy exercise lessons and videos about various disease and health condition
Decerebrate posturing (decerebrate rigidity, abnormal extensor reflex)
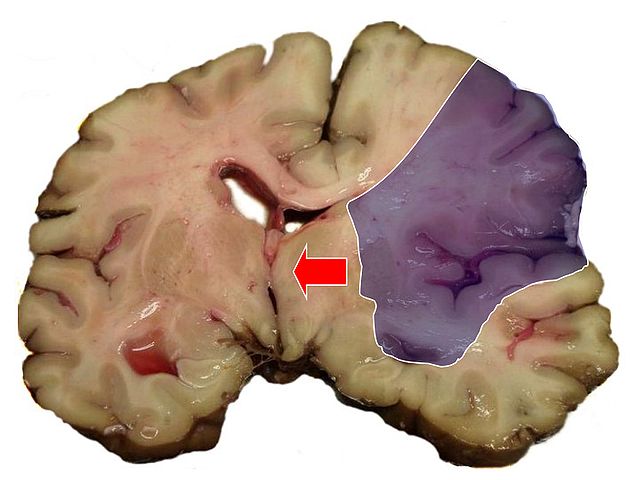
Decerebrate posturing (decerebrate rigidity, abnormal extensor reflex) is characterized by adduction and extension of the arms, with the wrists pronated and the fingers flexed. The legs are stiffly extended, with plantar flexion of the feet. In severe cases, the back is acutely arched (opisthotonus). (See Recognising decerebrate posture.) This sign indicates upper brain stem damage, which may result from primary lesions, such as infarction, hemorrhage or tumor; metabolic encephalopathy; head injury; or brain stem compression associated with increased intracranial pressure (ICP). This postural pattern was first described by Sherrington, who produced it in cats and monkeys by transecting the brainstem at the intercollicular level.
Alert
If you observe decerebrate rigidity/posture:
- Ensure a patent airway.
- Turn the patient’s head to the side to prevent aspiration (Don’t disrupt spinal alignment if you suspect spinal cord injury.)
- Examine spontaneous respirations, and institute emergency measures if necessary.
- After the patient has stabilized, perform a focussed assessment.
Decerebrate rigidity may be elicited by noxious stimuli or may occur spontaneously. It may be unilateral or bilateral. With concurrent brain stem and cerebral damage, decerebrate rigidity may affect only the arms, with the legs remaining flaccid. Alternatively, decerebrate rigidity may affect one side of the body and decorticate rigidity the other. The two postures may also alternate as the patient’s neurologic status fluctuates. Generally, the duration of each posturing episode correlates with the severity of brain stem damage.
History
- Explore the history of the patient’s coma. If you can’t obtain this information, look for clues to the causative disorder, such as hepatomegaly, cyanosis, diabetic skin changes, needle tracks, or obvious trauma.

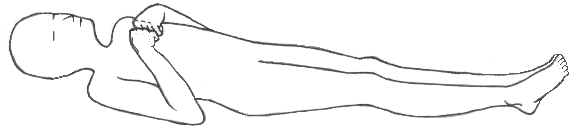
RECOGNISING DECEREBRATE POSTURing
Decerebrate rigidity/posture results from damage to the upper brain stem. In this posture, the arms are adducted and extended, with the wrists pronated with the fingers flexed. The legs are stiffly extended, with plantar flexion of the feet.
- Ask the patient’s family when his level of consciousness (LOC) began deteriorating. Did it occur abruptly? What did the patient complain of before he lost consciousness?
- Review the patient’s medical history for diabetes, liver disease, cancer, blood clots, or aneurysm.
- Ask the patient’s family about an incident or trauma that could be responsible for the coma.
PHYSICAL ASSESSMENT
- Take the patient’s vital signs, and determine his LOC; use the Glasgow Coma Scaleas a reference. Be alert for signs of increased ICP (such as bradycardia, increasing systolic blood pressure, and widening pulse pressure) and neurologic deterioration (such as altered respiratory pattern and abnormal temperature).
- Evaluate the pupils for size, equality and response to light.
- Assess deep tendon and cranial nerve reflexes, and test for doll’s eye sign.
SPECIAL CONSIDERATIONS
Relief of high ICP by removal of spinal fluid during a lumbar puncture may precipitate cerebral compression of the brain stem and cause decerebrate posture and coma.
PEDIATRIC POINTERS
- Children younger than age 2 may not display decerebrate rigidity/posture because of the immaturity of their central nervous system. However, if the posture does occur, it’s usually the more severe opisthotonos. In fact, opisthotonos are more common in infants and young children than in adults and is usually a terminal sign.
- In children, the most common cause of decerebrate posture is head injury. It also occurs with Reye’s syndrome- the result of increased ICP causing brain stem compression.
PATIENT COUNSELLING
Inform the patient’s family that decerebrate posture is a reflex response, not a voluntary response to pain or a sign of recovery. Offer emotional support.
similar pages
References
- Rapid Assessment: A Flowchart Guide to Evaluating Signs and Symptoms- By Lippincott Williams & Wilkins
- Clinical Neurology 5th edition (February 9, 2002): by David A. Greenberg, Michael J. Aminoff, Roger P. Simon By McGraw-Hill/Appleton & Lange
- ADAMS AND VICTOR’S PRINCIPLES OF NEUROLOGY 8th 2005
Back to home page
Recent Articles
|
Author's Pick
Rating: 4.4 Votes: 252 |